
Reviewed By: Barbara Rexer, DSW, LCSW, LCADC, CCS, ICCS, DRCC
Most people know that drinking can temporarily affect your brain. But if you abuse alcohol for a long period of time, the risk of long-term damage rises significantly. One potential outcome is “wet brain,” a condition that can lead to fatigue, confusion and amnesia. Here's what you need to know.
Table Of Contents
What Is “Wet Brain” Syndrome?
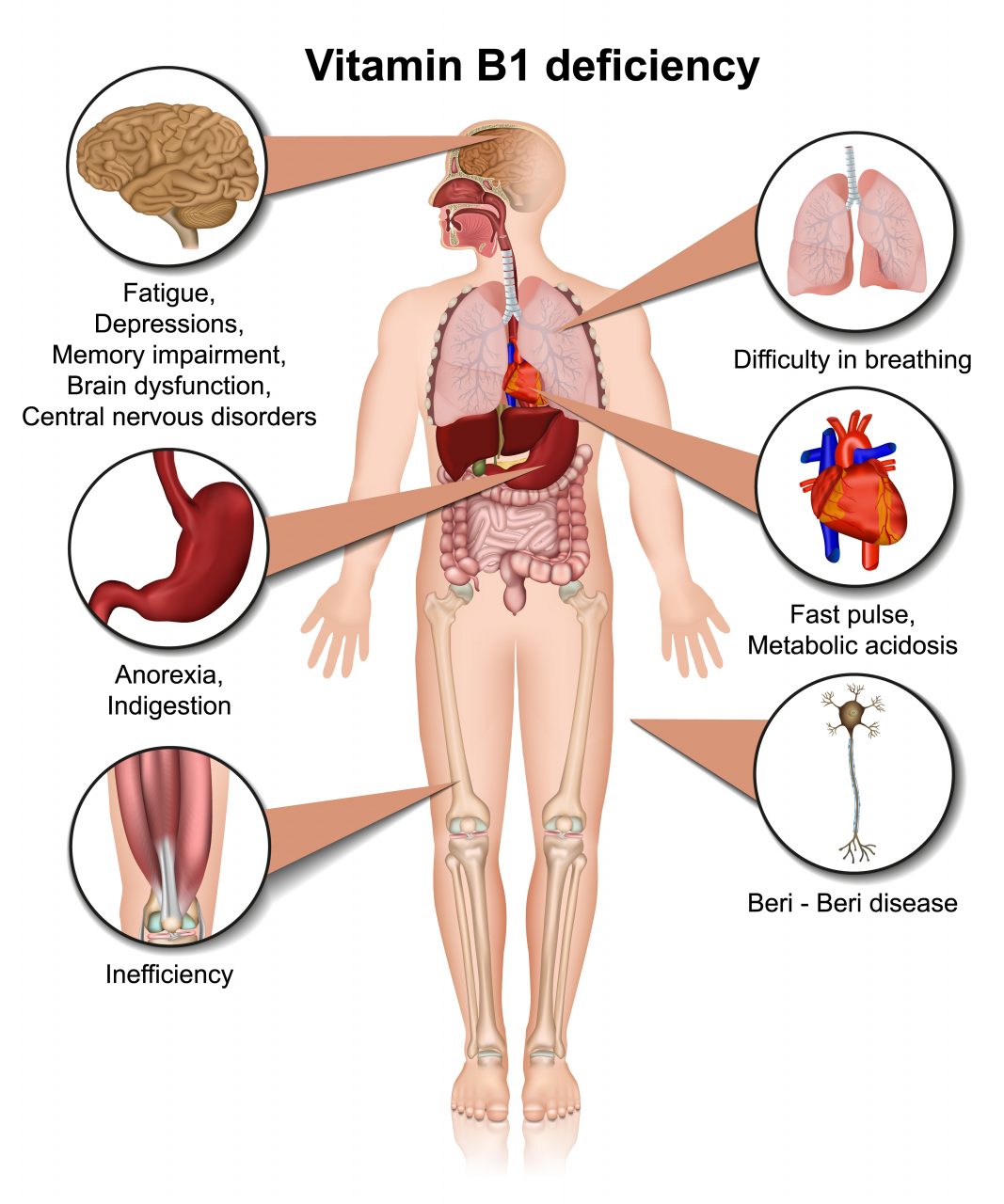
Wet brain, also known as Wernicke-Korsakoff syndrome, is a form of cognitive impairment caused by a lack of vitamin B1 (thiamine). It primarily affects people who struggle with long-term alcohol use disorder (AUD). Although most people get enough thiamine through the foods they eat, those who struggle with alcohol often lack nutrients in their diets. As a result, even if they consume enough calories, long-term alcohol users may be deficient in important vitamins and minerals.
Other factors related to drinking can also increase the risk of developing wet brain. For example, a lack of appetite or frequent vomiting can limit the amount of thiamine consumed or prevent it from being absorbed. Moreover, long-term damage to the liver harms the body’s ability to store thiamine, even on a small scale. All of these situations can lead to a thiamine deficiency.
What Are the Symptoms?
Wet brain appears in stages, each with its own set of symptoms. Early on, physical symptoms may include:
- Anemia or other co-occurring nutritional deficiencies
- Eyelid drooping
- Fatigue or weakness
- Leg twitches or spasms
- Loss of appetite
- Memory loss
- Nausea
- Nutrition decline
- Rapid weight loss
- Vomiting
In the early stages, those who suffer may appear confused or have trouble concentrating. You might also notice personality changes, short-term memory issues, talkativeness or a propensity to tell fantastical stories — the result of the brain “filling in the gaps” of memory loss.
As the condition progresses, severe symptoms develop. These may include:
- Abnormal eye movements
- Slurred speech
- Brain swelling
- Physical weakness
- Dementia
- Diminishing mental capacity
- Double vision
- Peripheral neuropathy
- Polyneuropathy
- Postural hypotension
- Severe confusion
- Syncope
- Tachycardia
Later stages also involve ataxia, or a degenerative disease of the nervous system. As this progresses, a person may lose a substantial amount of muscle tone. It might begin as a lack of coordination, similar to drunkenness, and gradually evolve into an inability to stand or walk unassisted.
Preventing Wet Brain Syndrome
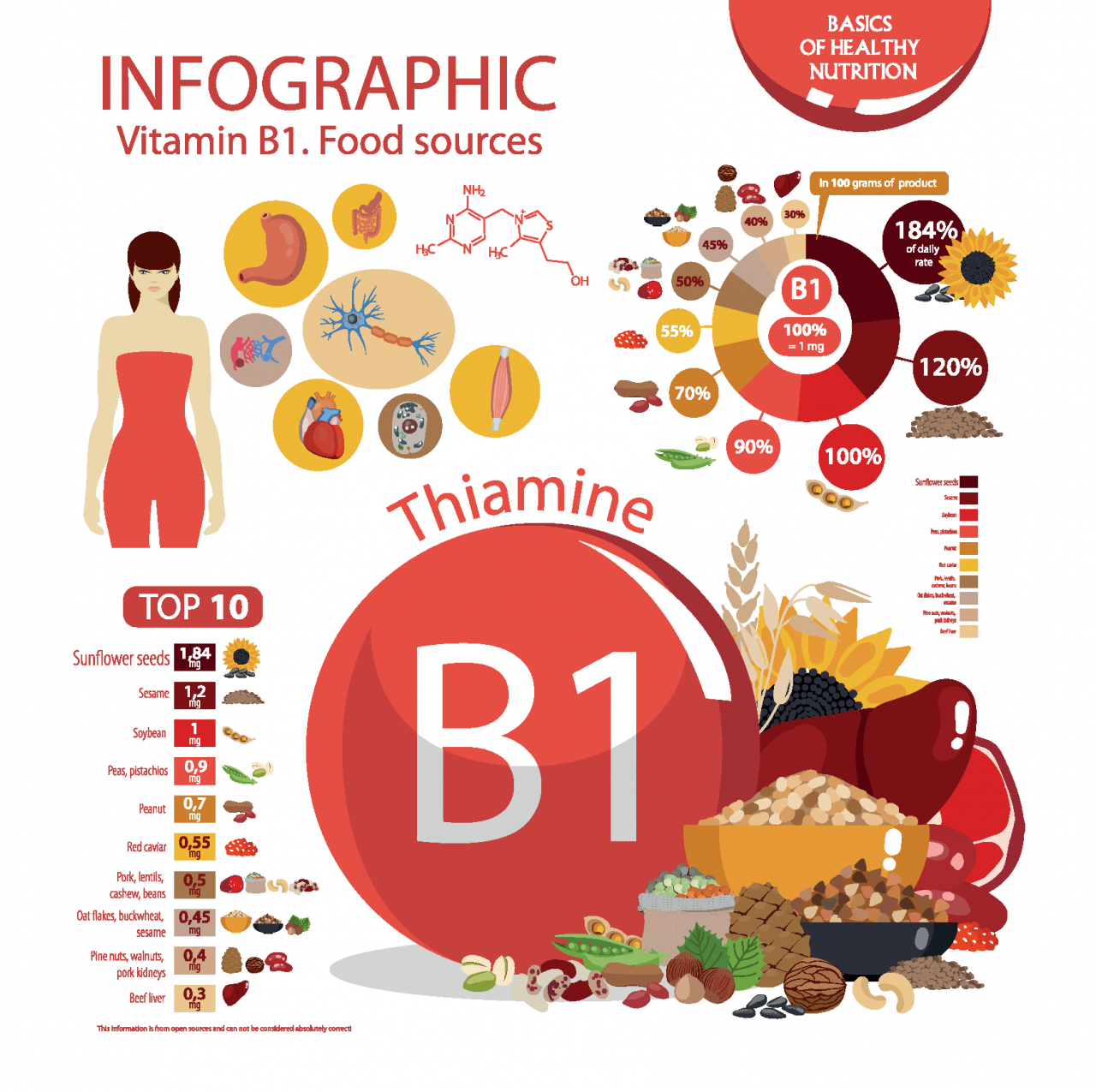
Since wet brain is the result of a thiamine deficiency, the most direct way to prevent the condition is to simply get enough vitamin B1. This starts with your diet. Below are foods rich in vitamin B1 to help boost your thiamine.
However, addressing the deficiency alone does not solve the core problem. Preventing wet brain syndrome starts with preventing long-term alcohol abuse. This means watching for signs that a loved one is struggling, or recognizing a need for treatment yourself. Having the courage to seek help is the most practical and effective way to prevent wet brain syndrome.
Treatment
Treatment for wet brain syndrome typically begins with a thiamine supplement. If you cannot ingest it orally, your doctor might administer it intravenously or intramuscularly. However, this only treats your body’s need for vitamin B1. Once Wernicke-Korsakoff syndrome sets in, existing brain damage or memory loss can be permanent. Treatment can only slow the disease’s progression.
This is why it’s so important to seek treatment if you suspect your alcohol use has become a problem. The earlier you start your path toward recovery, the greater chance you have of preventing long-term damage.
Other Effects of Long-Term Alcohol Use
Long-term alcohol exposure impacts the mind and body in a number of ways. It can cause the frontal lobes of the brain to shrink, resulting in cognitive impairments. Behavioral changes and memory issues can also develop. Some people experience hallucinations.
Chronic heavy drinking typically leads to cardiovascular, pancreas, and liver disease. Additionally, long-term problem drinkers are more likely to develop lung infections and cancer.
Thinning bones, stomach distress, sexual dysfunction, and infertility are all potential side effects of long-term alcohol use. Diabetes complications and numbness are possible, as well as muscle cramps and muscle death.
Over time, you may also become dependent on alcohol. Ultimately, it impairs your ability to function mentally, physically, and socially.
How to Help a Loved One with Long-Term Alcohol Addiction
There are many ways to help a loved one who is suffering from long-term alcohol addiction. Inpatient treatment is often ideal because of the serious withdrawal symptoms associated with alcohol. If you have a co-occurring mental health disorder or medical issue, inpatient treatment can also provide a safe environment under the supervision of medical professionals. However, many flexible outpatient options exist as well. If you are generally healthy and have a strong support system, intensive outpatient programs are good options.
After the detox phase, it is important to continue steps toward recovery. Cognitive behavioral therapy is a common path that helps you develop coping mechanisms to manage triggers or negative thought patterns. Many people also find success with 12-step meetings and other support groups. The key is to find what works for you and to continue seeking support when you need it.
Have questions about addiction?Chat with one of our recovery specialists now.

Written By: Sprout Editorial Team
The Sprout Health Group editorial team is passionate about addiction treatment, recovery and mental health issues. Every article is expert-reviewed.


